TRITIYA SOPAN
TRITIYA SOPAN TESTING CAMP
TRITIYA SOPAN TESTING CAMP – REQUIREMENTS
WHAT TO BRING?
1. GOOD TURN DIARY (WRITTEN FOR ATLEAST A MONTH)
2. GENERAL LOG BOOK ( WRITTEN FOR PRAVESH, PRATHAM SOPAN, DWITIYA SOPAN AND TRITIYA SOPAN)
3. ACTIVITY NOTEBOOK/NOTEBOOKS
( PRATHAM SOPAN – 02 ACTIVITIES
DWITIYA SOPAN – 02 ACTIVITIES
TRITIYA SOPAN – 01 ACTIVITY)
4. PROFICIENCY NOTEBOOKS
DWITIYA SOPAN – 01 PROFICIENCY BADGE
TRITIYA SOPAN – SWIMMING / 01 PROFICIENCY BADGE AND
TWO OTHER PROFICIENCY BADGES
5. DATE OF BIRTH CERTIFICATE
6. INFORMATION SHEET CONTAINING THE FOLLOWING:
A.NAME OF THE VIDYALAYA
B.NAME OF THE GROUP
C. GROUP REGISTRATION NUMBER
D. NAME OF THE TROOP
E. NAME OF THE SCOUT
F.DATE OF BIRTH
G. DATE OF PASSING PRAVESH
H. DATE OF INVESTITURE
I.DATE OF PASSING PRATHAM SOPAN
J.DATE OF PASSING DWITIYA SOPAN
K.DETAILS OF ACTIVITIES UNDERTAKEN AT ALL LEVELS
L.DETAILS OF PROFIENCY BADGES DONE ( WITH THE NAME OF THE EXAMINER, DATE OF EXAMINATION)
M.NAME OF THE SCOUTMASTER WITH DESIGNATION IN SCOUTING AND WARRANT NUMBER
N. DATE OF COH RECOMMENDATION
O.SIGNATURE OF THE SCOUT
P. SIGNATURE OF THE PARENT/GUARDING
Q. SIGNATURE OF THE PRINCIPAL WITH SEAL
7. TWO PASS PORT SIZE PHOTOS IN UNIFORM
8.KNOTTING ROPE
9. LASHING ROPE
10. BANDAGE CLOTH
11. CORRECT AND COMPLETE UNIFORM 02 SETS
12. ONE ROUGH NOTE FOR TAKING POINTS FOR FURTHER PROGRESS IN THE MOVEMENT
Pioneering projects
Pioneering projects
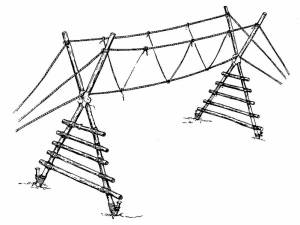
Simple Ladder Bridge – Pioneering for the Scouts

Equipment
– 6 x spars 3.6m to 5m (12 to 16ft) long
– 6 x spars 2.5m (8ft) long
– 2 x spars 2m (6ft long)
– light spars for ladder rungs
– lashing lengths
– large pegs or pickets
Method
Start by making a tripod on each side of the stream/gully using two long spars and a shorter one that will be the back leg. The actual lengths of the spars will depend on the depth of the stream etc. Use either a figure of eight or a tripod lashing.
Lash horizontal spars across the long legs to form and A frame. They should be positioned so that they will be slightly higher than the bank when the legs are placed in their final positions.
Place the longer legs in the stream so that they have firm footings and are on line. Pull the shorter legs back until they are stable.
Drive a picket into the ground alongside and at right angles to the back spar and lash the two together.
The footways are ladders made from light spars lashed along longer spars. For additional strength fix the rungs on top of their supports. The ladder for the central span should be a good fit inside the A frame. The outer ladders should be narrower so that they will fit inside the centre ladder. It may be necessary to tie the ladders to the A frames to ensure they do not slip.
Finally, fit two hand ropes between the tripods as shown in the diagram.
PIONEERING PROJECTS
PIONEERING PROJECT
MONKEY BRIDGE
Equipment
– 4 x spars 3.6m long
– 2 x spars 2m long
– 8 – 10 light spars for ladder rungs
– lashing lengths
– Additional light lines 2 – 3m long
– 3 hawsers 20 – 24m long
– 1 pulley suitable for hawsers
– 1 Handy Billy
– sisal
– sacking
– large pegs or pickets
MethodThis bridge will require substantial ground anchors at each end. Before you start building, check to see if there are any suitable trees to act as anchors. If you do use trees, do not forget to protect them from abrasion by wrapping them in sacking.Construct 2 A frames by laying 2 x 3.6m spars alongside each other and tying a sheer lashing approx 1 1/2m from the top. Open the spars out and lash a 2m spar across the base, using square lashings.Lash light spars above the base to form a simple ladder.To protect the ropes, place some sacking in the crutch of the frame and secure it in place with sisal.Tie guy ropes to the top of the spars.To make the walkway, lay the foot rope on the ground and mark the approximate position of the A frame.Place the hand rope about 1.25m either side of the foot rope. It is a good idea to peg these ropes down to maintain the spacing during the next stage.Using the light line (6mm polypropylene is ideal) attach the middle to the foot rope with a clove hitch and the ends to the hand ropes with a round turn and two half hitches. The bridge will require a vee rope every metre or so.With the A frames in position, but still on the ground, check the alignment of the bridge – the frames must be in a straight line between the ground anchors/trees.Anchor one end of the foot rope using a round turn and two half hitches and fit a Handy Billy to the other.Raise one A frame at a time and guy them when they are upright. Heel the butts into the ground to stop them sliding during use.As you tension the foot rope, use a light spar to ease it over the A frame otherwise it will lock in the crutch and tend to pull the frame over. Make the other end of the rope off and remove the Handy Billy.The bridge should now be strong enough to allow the A frames to be climbed. Attach the hand ropes to the top of the spars using a loose square lashing. Tension them off using the Handy Billy and then tighten the lashings with a couple of frapping turns.NoteThe tension in the hand ropes must be the same. This can be achieved either by using a very long rope doubled back on itself or by looping the two ropes together and placing a sing large pulley block in that loop. The ropes are tensioned with the Handy Billy attached to this block.
– 2 x spars 2m long
– 8 – 10 light spars for ladder rungs
– lashing lengths
– Additional light lines 2 – 3m long
– 3 hawsers 20 – 24m long
– 1 pulley suitable for hawsers
– 1 Handy Billy
– sisal
– sacking
– large pegs or pickets
MethodThis bridge will require substantial ground anchors at each end. Before you start building, check to see if there are any suitable trees to act as anchors. If you do use trees, do not forget to protect them from abrasion by wrapping them in sacking.Construct 2 A frames by laying 2 x 3.6m spars alongside each other and tying a sheer lashing approx 1 1/2m from the top. Open the spars out and lash a 2m spar across the base, using square lashings.Lash light spars above the base to form a simple ladder.To protect the ropes, place some sacking in the crutch of the frame and secure it in place with sisal.Tie guy ropes to the top of the spars.To make the walkway, lay the foot rope on the ground and mark the approximate position of the A frame.Place the hand rope about 1.25m either side of the foot rope. It is a good idea to peg these ropes down to maintain the spacing during the next stage.Using the light line (6mm polypropylene is ideal) attach the middle to the foot rope with a clove hitch and the ends to the hand ropes with a round turn and two half hitches. The bridge will require a vee rope every metre or so.With the A frames in position, but still on the ground, check the alignment of the bridge – the frames must be in a straight line between the ground anchors/trees.Anchor one end of the foot rope using a round turn and two half hitches and fit a Handy Billy to the other.Raise one A frame at a time and guy them when they are upright. Heel the butts into the ground to stop them sliding during use.As you tension the foot rope, use a light spar to ease it over the A frame otherwise it will lock in the crutch and tend to pull the frame over. Make the other end of the rope off and remove the Handy Billy.The bridge should now be strong enough to allow the A frames to be climbed. Attach the hand ropes to the top of the spars using a loose square lashing. Tension them off using the Handy Billy and then tighten the lashings with a couple of frapping turns.NoteThe tension in the hand ropes must be the same. This can be achieved either by using a very long rope doubled back on itself or by looping the two ropes together and placing a sing large pulley block in that loop. The ropes are tensioned with the Handy Billy attached to this block.
PIONEERING PROJECTS
PIONEERING PROJECTS
Banana Bridge
Equipment
– 20 x 1.8m (6ft) spars
– 5 x 2.4m (8ft) spars
– 8 x 3.0m (10ft) spars
– 4 x 4.0m (12ft) spars
– 4 x 5.0m (16ft) spars
– 68 lashing lengths
– 6 long ropes
– large tent pegs
– 4 stout pickets
– 1 maulMethodConstruct 4 pairs of sheer legs using 8 x 3m (10ft) spars and sheer lashings – two on each side of your stream or ravine.Lean the sheer legs together in pairs to form two low pyramidsLash the 5m (16ft) spars across the long sides of each pyramid.Lash 2.4m (8ft) spars across the short side of each pyramid to provide stability during assembly.Prepare a ‘trapeze’ to support the centre of the walkway by tying a lashing length to each end of the remaining 2.4m spar with a round turn and two half hitches. Tie the other end of the lashing lengths to the corners of one of the pyramids at A and B.Tie a long rope to the corners of the pyramid next to the trapeze ropes. These will be used to raise the pyramid into position.Ease the pyramid forward across the stream, lifting it using the long ropes and manoeuvering the corners on the ground into position. Place large pegs in the ground to prevent the corners sliding. Lift it higher then the finished structure will require and tie off the long ropes to pickets to stabilise it.Place the other half of the bridge in line with the first, tie two long ropes to the corners and raise it, maneuvering it into position and putting in pegs around the bottom corners.With a team of Scouts on either side, gently lower the pyramids until they interlock.Lash the 12ft spars together to form the sides of the walkway. Lash the 1.8m (6ft) spars across these to make a ladder.Carefully pass the ladder across the stream and through the trapeze so that either end rests on the bank.Helpful hintCareful measurement is required to ensure that the pyramids are the correct distance apart – this may only be resolved through trial and error. Too far apart and they will not lock but will fall down – too close and they may fall backwards.Knock pegs into the banks and lash the ends of the ladder to them to ensure they do not slip. Finally, tie ropes between the pyramids to act as hand rails
– 20 x 1.8m (6ft) spars
– 5 x 2.4m (8ft) spars
– 8 x 3.0m (10ft) spars
– 4 x 4.0m (12ft) spars
– 4 x 5.0m (16ft) spars
– 68 lashing lengths
– 6 long ropes
– large tent pegs
– 4 stout pickets
– 1 maulMethodConstruct 4 pairs of sheer legs using 8 x 3m (10ft) spars and sheer lashings – two on each side of your stream or ravine.Lean the sheer legs together in pairs to form two low pyramidsLash the 5m (16ft) spars across the long sides of each pyramid.Lash 2.4m (8ft) spars across the short side of each pyramid to provide stability during assembly.Prepare a ‘trapeze’ to support the centre of the walkway by tying a lashing length to each end of the remaining 2.4m spar with a round turn and two half hitches. Tie the other end of the lashing lengths to the corners of one of the pyramids at A and B.Tie a long rope to the corners of the pyramid next to the trapeze ropes. These will be used to raise the pyramid into position.Ease the pyramid forward across the stream, lifting it using the long ropes and manoeuvering the corners on the ground into position. Place large pegs in the ground to prevent the corners sliding. Lift it higher then the finished structure will require and tie off the long ropes to pickets to stabilise it.Place the other half of the bridge in line with the first, tie two long ropes to the corners and raise it, maneuvering it into position and putting in pegs around the bottom corners.With a team of Scouts on either side, gently lower the pyramids until they interlock.Lash the 12ft spars together to form the sides of the walkway. Lash the 1.8m (6ft) spars across these to make a ladder.Carefully pass the ladder across the stream and through the trapeze so that either end rests on the bank.Helpful hintCareful measurement is required to ensure that the pyramids are the correct distance apart – this may only be resolved through trial and error. Too far apart and they will not lock but will fall down – too close and they may fall backwards.Knock pegs into the banks and lash the ends of the ladder to them to ensure they do not slip. Finally, tie ropes between the pyramids to act as hand rails
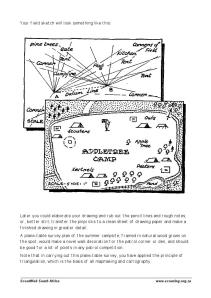
PLANE TABLE METHOD OF MAP MAKING
TRIANGULATION METHOD OF MAP MAKING
FRACTURE: ARM AND COLLARBONE
Open and Closed Fractures and How to Treat Them
There are two classifications of fractures, closed fractures and open fractures. Closed fractures include any fracture where the bone does not penetrate the skin (the skin stays closed). In such instances, proper treatment includes immobilizing the fracture and seeking medical help.
Open fractures occur when a bone or bone fragment breaks through the skin or the skin and bone are broken in a traumatic, crushing injury. Proper treatment for open fractures must also include concern for possible infection.
Recognizing Fractures:
An open fracture will typically be self evident due to the exposed bone. The following clues suggest you are dealing with a probable closed fracture:
- The victim felt a bone break or heard a “snap”.
- The victim feels a grating sensation when he/she moves a limb. (This condition is known as crepitus.)
- One limb appears to be a different length, shape or size than the other, or is improperly angulated.
- Reddening of the skin around a fracture may appear shortly after the fall.
- The patient may not be able to move a limb or part of a limb (e.g., the arm, but not the fingers), or to do so produces intense pain.
- Loss of a pulse at the end of the extremity.
- Loss of sensation at the end of the extremity.
- Numbness or tingling sensations.
- Involuntary muscle spasms.
- Other unusual pain, such as intense pain in the rib cage when a victim takes a deep breath or coughs.
If you discover any of these symptoms and cannot attribute them to any other obvious cause, assume them to be a fracture.
Initial Care for Fractures
In treating fractures, an unhurried and careful approach is best. Few fractures are life threatening unless mishandled. Check the patient for any more serious injuries. Make sure someone is going for help, or call 911. Ensure your patient is breathing and that excessive bleeding is controlled and that all open wounds are protected as best you can from contamination. After these elements are satisfied you can deal with stabilization of the fracture.
If you can, carefully cut away all clothing near the fracture site. You need to make sure the fracture hasn’t broken the skin and you may be able to use the cut away material to aid in splinting. If you find an open fracture, protect the wound from contamination as you would any other.
No matter how soon you expect to get medical help, you should immobilize all fractures to prevent additional injuries due to accidental movement or muscle spasms. Immobilization can be achieved many ways; the key points being not to worsen the situation while immobilizing and making sure to also immobilize the joints above and below any limb fracture.
DO NOT try to straighten angulations of a bent wrist, ankle or shoulder or attempt to straighten any dislocated joint!
When splinting using sticks or other “found” objects, try to make padding between the injured limb and splint using a jacket, shirt filled with grass, anything which can be reasonably secured and can help fill in the gaps between the limb and the splint material. Don’t get carried away with this concept, but if you can handily make something up without delaying the splinting process, it will be more comfortable to the patient.
It is not always possible to tell with the naked eye if a bone has been fractured. In case of doubt, it is best to assume the victim has received a fracture and treat it accordingly.
First Aid to Arm, and Collarbone Fractures
Collarbone Fractures:
| A collarbone fracture is commonly caused by indirect force resulting from a fall on an outstretched hand or the point of the shoulder. | |
| Collarbone fracture due to a direct force are rare. |
Symptoms and Signs:
| General symptoms and signs of fracture. | |
| Casualty may support the arm on the injured side at the elbow and may keep the head inclined towards the injured side to relieve pain. |
Treatment:
- Gently place the limb on the injured side across the casualty’s chest with the fingertips almost resting on the opposite shoulder.
- Place padding between the limb and chest on the affected side.
- Support the limb and padding in an elevation sling.
- For additional support, secure the limb to the chest by applying aboard bandage over the sling, tie the knot in front on the uninjured side.
- Remove to hospital.
Arm Fractures:
Fractures can occur anywhere along the length of the upper-arm bone or the two forearm bones, and may involve the elbow and upper arm bone.
Treatment:
- Place a pad in the person’s armpit.
- Use a padded splint.
- Support the lower arm with a narrow pad around the neck and wrist.
- Use a wide bandage to bind the upper arm to the chest.
JAW FRACTURE
JAW FRACTURE
The term “jaw fracture” usually refers to fracture of the lower jaw (mandible). A fractured jaw causes pain and usually changes the way the teeth fit together. Often, the mouth cannot be opened wide, or it shifts to one side when opening or closing.
Fractures of the upper jaw (maxilla) are usually considered facial fractures. These may cause double vision (because the muscles of the eye attach nearby), numbness in the skin below the eye (because of injuries to nerves), or an irregularity in the cheekbone that can be felt when running a finger along it.
Any injury forceful enough to fracture the jaw may also injure the spine in the neck or cause a concussion or bleeding within the skull. Jaw fractures cause swelling, which rarely becomes severe enough to block the airway. Sometimes a fracture extends through a tooth or its socket (called an open fracture), creating an opening into the mouth that can allow oral bacteria to infect the jaw bone.
If people suspect their jaw is fractured, they should hold the jaw still with the teeth together. Emergency personnel may wrap a bandage under the jaw and over the top of the head several times (Barton’s bandage). When wrapping the bandage, people must be careful not to cut off breathing.
Symptoms of Jaw Fracture
Symptoms include Pain in the face or jaw, located in front of the ear on the affected side(s), worse with movement, inability to close your mouth, drooling because of inability to close the mouth. difficulty speaking, jaw may protrude forward, your teeth may not align normally, your ite feels “off” or crooked
Causes of Jaw Fracture
The most common cause of broken or dislocated jaw is accident or trauma involving a blow to the face. This may be the result of a motor vehicle accident, industrial accident, recreational/sports injury, or other accident. It may also result from assault. The goal of treatment is proper alignment of the jaw bone so the upper and lower teeth come together normally. Surgery is often required for moderate to severe fractures to align and immobilize the bone so it can heal.
Treatment of Jaw Fracture
Treatment for conservative Jaw Fracture
This means that patients whose fracture does not affect mastication must rest the areas of the broken bone. This usually includes unfitness for work, the duration of which will be determined by the treating doctor.
In fractures affecting the jaws, immobilisation of the jaws is necessary for conservative treatment, and this can be ensured by retaining screws or encirclement of the teeth with strong wire.
In fractures affecting the jaws, immobilisation of the jaws is necessary for conservative treatment, and this can be ensured by retaining screws or encirclement of the teeth with strong wire.
Operative therapy
If operative treatment is necessary, this involves an operation that is usually performed under general anaesthesia. The broken fragments of bone are exposed at the operation and the fractured parts of the bone are joined together firmly in their original position using plates and screws. Various systems are available depending on the fracture site and fracture type: titanium plate systems are used in fractures subject to much stress, especially in the mandible, while absorbable plate systems (dissolving plates) can be used in fractures in less stressed areas, especially in the maxilla and zygomatic area and in the frontal region. The treating doctor decides on the procedure and treatment plan in each case.
The fundamental goals of treatment are restoration of the original form and function, facial shape and mastication. This eliminates pain caused by the fracture and diminishes the risk of infection with its possible sequelae (chronic bone inflammation).
Treatment of Jaw Fracture
Treatment for conservative Jaw Fracture
This means that patients whose fracture does not affect mastication must rest the areas of the broken bone. This usually includes unfitness for work, the duration of which will be determined by the treating doctor.
In fractures affecting the jaws, immobilisation of the jaws is necessary for conservative treatment, and this can be ensured by retaining screws or encirclement of the teeth with strong wire.
In fractures affecting the jaws, immobilisation of the jaws is necessary for conservative treatment, and this can be ensured by retaining screws or encirclement of the teeth with strong wire.
Operative therapy
If operative treatment is necessary, this involves an operation that is usually performed under general anaesthesia. The broken fragments of bone are exposed at the operation and the fractured parts of the bone are joined together firmly in their original position using plates and screws. Various systems are available depending on the fracture site and fracture type: titanium plate systems are used in fractures subject to much stress, especially in the mandible, while absorbable plate systems (dissolving plates) can be used in fractures in less stressed areas, especially in the maxilla and zygomatic area and in the frontal region. The treating doctor decides on the procedure and treatment plan in each case.
The fundamental goals of treatment are restoration of the original form and function, facial shape and mastication. This eliminates pain caused by the fracture and diminishes the risk of infection with its possible sequelae (chronic bone inflammation).
COLLARBONE FRACTURE
FRACTURE
FRACTURE
A fracture is a broken bone. It requires medical attention. If the broken bone is the result of major trauma or injury, call your local emergency number. Also call for emergency help if:
- The person is unresponsive, isn’t breathing or isn’t moving. Begin cardiopulmonary resuscitation (CPR) if there’s no respiration or heartbeat.
- There is heavy bleeding.
- Even gentle pressure or movement causes pain.
- The limb or joint appears deformed.
- The bone has pierced the skin.
- The extremity of the injured arm or leg, such as a toe or finger, is numb or bluish at the tip.
- You suspect a bone is broken in the neck, head or back.
- You suspect a bone is broken in the hip, pelvis or upper leg (for example, the leg and foot turn outward abnormally).
Don’t move the person except if necessary to avoid further injury. Take these actions immediately while waiting for medical help:
- Stop any bleeding. Apply pressure to the wound with a sterile bandage, a clean cloth or a clean piece of clothing.
- Immobilize the injured area. Don’t try to realign the bone or push a bone that’s sticking out back in. If you’ve been trained in how to splint and professional help isn’t readily available, apply a splint to the area above and below the fracture sites. Padding the splints can help reduce discomfort.
- Apply ice packs to limit swelling and help relieve pain until emergency personnel arrive. Don’t apply ice directly to the skin — wrap the ice in a towel, piece of cloth or some other material.
- Treat for shock. If the person feels faint or is breathing in short, rapid breaths, lay the person down with the head slightly lower than the trunk and, if possible, elevate the legs.
Fractures
A fracture is a complete or partial breakage of a bone. Fractures may be:
- Simple, where the broken ends of the bone do not cut open the skin
- Compound, where the broken end of the bone may be in contact with the external air
- Complicated, where in addition to the fracture an important internal organ may also be injured. A complicated fracture may also be simple or compound.
Signs and Symptoms of a Fracture
- Pain at or around the site of the fracture.
- Tenderness (pain on gentle pressure) over the area. Do not press hard.
- Swelling over the area with discoloration.
- Loss of normal movements of the affected part.
- Deformity of the limb may be caused. The limb may lose its normal shape and there may be apparent shortening of the limb.
- If, as in the leg bone, the break is just under the skin, the irregular outline of the bone can be felt easily.
- When one end of the broken bone moves against the other, a crackling sound may be heard. This is called crepitus (grating). This should never be elicited by the person giving First Aid.
- Unnatural movements may be felt at the site of the fracture. This too should never be elicited by the First-Aid provider.
In addition the victim may himself say that he heard the snap of the bone. It is important to compare the injured limb with the normal limb while making an assessment.
Management of Fractures
The aims of First Aid here are:
- To prevent further damage
- To reduce pain
- To make the patient feel comfortable
- To get medical aid as soon as possible
- Fractures often occur along with other injuries. So the rescuer must assess for other injuries and decide which of them requires care on priority. Heavy bleeding is more urgent and requires higher priority care over a fracture.
- If there is no danger to life then temporary attention to the fracture is often sufficient.
- Handle the patient very gently. Avoid all unnecessary movement.
- Treat for shock if present.
- If the broken ends of the bones show out, do not wash the wound or apply antiseptics to the end of the bone.
- Do not handle the fracture unnecessarily.
- Never attempt to reduce the fracture or to bring the bones to the normal position.
- Stabilise and support the injured part so that no movement is possible. This stops further injury and helps to control the bleeding.
- Immobilise the fracture area and the joints on both sides of the fracture site (above and below) by using bandages or by using splints wherever available. It is essential that the rescuer be familiar with the use of bandages and splints.
A: Using Bandages
Usually it is enough to use the other (uninjured) limb or the body of the victim as the splint. The upper limb can be supported by the body, and the lower limb by the other limb provided that also is not fractured. Most fractures except those of the forearm can be immobilised in this manner:
- Do not apply bandage over the area of the fracture.
- The bandaging should be firm so that there is no movement of the fractured ends but should not be too tight as blood circulation to the affected area could be reduced. If there is further swelling of the injured area, the bandage may be too tight and therefore may need to be loosened.
- Always place padding material between the ankles, knees and other hollows if they have to be tied together so that when the limbs are bound together they are comfortable and steady.
- If the patient is lying down, the bandage should be passed through the natural hollows like the neck, the lower part of the trunk, knees, just above the ankles etc., so that the patient’s body is not jarred.
- Always tie the knots on the sound side.
B: Using Splints
Splints are used only when necessary expertise is there.
- A splint is a rigid piece of wood or plastic material or metal applied to a fractured limb to prevent movement of the broken bone.
- Reasonably wide splints are better than narrow ones.
- Splints should be long enough so that the joints above and below the fractured bones can be made immobile.
- The splints should be well padded with cotton or cloth so as to fit snugly and softly on the injured limb.
- Splints are best applied over the clothing.
- In an emergency, splints can be improvised using a walking stick, an umbrella, a piece of wood, a book or even a firmly folded newspaper.
- Use of splints becomes obligatory only when both legs or both thigh bones are broken.
Fractures involving the back (vertebral column) require special care. In such cases, the victim should not be allowed to get up. Further, movement must be avoided as much as possible and emergency medical help must be sought.








No comments:
Post a Comment